Diabetes is a family of diseases marked by high levels of glucose in the blood, or hyperglycemia. In the United States, the Centers for Disease Control and Prevention (CDC) estimates a total of 29.1-million individuals or 9.3-percent of the population have been diagnosed with diabetes. Type 1 diabetes is characterized by the absence of a hormone, secretion from the pancreas, an endocrine organ, while type 2 diabetes is characterized by resistance and is closely associated with being overweight or obese. Both types of diabetes may have multiple complications. Ten recommendations for diabetes health maintenance are…
Want diabetes content delivered straight to your inbox? Sign up for our Diabetes newsletter and receive exclusive news and articles written from our team of diabetes experts.
1. Hemoglobin A1C
Hemoglobin A1C is a lab test that can be used to diagnose or assess the treatment of diabetes. The test represents the average blood glucose level over the previous three months. It can reveal how well an individual has been controlling their diabetes. The test is usually performed at a laboratory, but some medical offices perform them in house. No special preparation is needed for the hemoglobin A1C test.
When used to diagnose diabetes, the following results indicate less than 5.7-percent: Normal (no diabetes), 5.7-percent to 6.4 percent: Pre-diabetes, and 6.5-percent or higher: Diabetes. When assessing control of diabetes, the American Diabetes Association (ADA) recommends a goal hemoglobin A1C below 7-percent. If an individual’s hemoglobin A1C is above 7-percent, it means their blood glucose is not very well controlled. The hemoglobin A1C test should be performed every 6-months if diabetes is controlled or every 3-months if diabetes is not controlled.
2. Review Results of Blood Glucose Monitoring
Most doctors recommend individuals with diabetes monitor their blood glucose levels, anywhere from once to four times per day. It is vital that individuals keep a log of their blood glucose levels and provide a copy to their doctor. The log can give doctors an indication of how well an individual’s diabetes is controlled.
The ADA suggests the following blood glucose targets for adult with diabetes, “Before a meal (pre-prandial blood glucose): 70- to 130-mg/dL, 1 – to 2-hours after a meal (postprandial blood glucose): Less than 180-mg/dL, of note, low blood glucose (hypoglycemia) is defined as less than 70-mg/dL.” Glucose monitors can be used on the fingertips, forearm, or thigh. Urine tests for glucose in the urine are not as accurate as blood glucose checks, and should be avoided. The cost of most glucose monitors and supplies are covered by health insurance.
3. Blood Pressure
Control of blood pressure (BP) is crucial in individuals with diabetes. A blood pressure should be obtained at every office visit. A normal BP is less than 120/80 millimeters of mercury (mmHg, which is the unit of measurement of BP). A BP of 121-139/81-89 mmHg is considered abnormal and puts a diabetic at increased risk for the development of hypertension, or high blood pressure. Hypertension is a common comorbidity, or coexisting condition, of diabetes.
A diabetic with a BP greater than 140/90 mmHg, on more than one occasion, meets the criteria for the diagnosis of hypertension. Lifestyle therapy for a diabetic with hypertension should entail a low sodium diet (less than 2,400 mg of sodium per day), exercise (30 minutes most days of the week), and weight loss (if overweight). The ADA recommends a target BP of less than 130/80 mmHg. Two or more medications may have to be used to meet BP treatment goals.
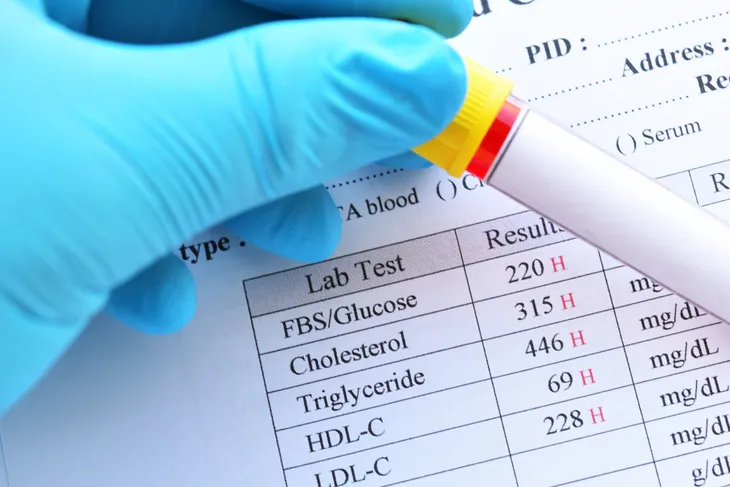
4. Fasting Lipid Panel
A fasting lipid, or cholesterol, panel can be used to diagnose elevated levels of cholesterol in the blood, or hyperlipidemia. Hyperlipidemia can contribute to ischemic heart disease in diabetics. A fasting lipid panel (FLP) consists of measurements for total cholesterol (TC), triglycerides (TG), LDL (“bad” cholesterol), and HDL (“good” cholesterol). An individual should be fasting (nothing to eat for 8- to 12-hours) when the cholesterol panel is drawn.
Recommended lifestyle therapy for a diabetic with hyperlipidemia is a low cholesterol diet, exercise (30 minutes most days of the week), and weight loss (if overweight). In those individuals not meeting treatment goals, a statin medication should be prescribed. A FLP should be obtained, on average, every 3- to 6-months. The ADA recommends the following lipid treatment goals for diabetics with hyperlipidemia: TC less than 200 mg/dL, LDL less than mg/dL, HDL greater than 40 mg/dL in men, HDL greater than 50 mg/dL in women, and TG less than 150 mg/dL.
5. Microalbuminuria Test
All individuals with diabetes should be screened for microalbuminuria at least once per year. The microalbuminuria test measures the amount of albumin, or protein, in the urine. Microalbuminuria can be screened for by the following three methods, 1. Random spot collection to measure albumin-to-creatinine ratio (preferred), 2. Timed collection, 3. 24-hour urine collection with serum creatinine
Microalbuminuria is abnormal and may be a sign of early kidney disease, or nephropathy. Diabetic nephropathy is damage to the kidneys caused by diabetes. Severe cases can lead to kidney failure. The mainstay of treatment for nonpregnant diabetics with microalbuminuria is control of blood pressure (BP) with medications such as angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs), which have the potential to prevent or slow the progression of kidney disease. The ADA suggests a goal target for microalbuminuria of less than 30 micrograms/mg creatinine.
6. Dilated and Comprehensive Eye Exam
All individuals with diabetes should screened for the presence of diabetic eye disease with a dilated and comprehensive eye exam at least once a year. Diabetic eye disease may include diabetic retinopathy, diabetic macular edema (DME), cataract, and glaucoma. Diabetic retinopathy is the most common cause of vision loss in individuals with diabetes. DME refers to swelling of the retina and is a consequence of diabetic retinopathy.
Adults with diabetes are two to five times more likely to develop cataracts (clouding of the lens of the eye) than adults who don’t have diabetes. In adults, diabetes nearly doubles the risk of glaucoma (damage to the optic nerve due to high pressure in the eye). The ADA recommends annual screening for the presence of retinopathy with a dilated and comprehensive eye exam administered by an ophthalmologist or optometrist. The ADA target would be normal, healthy eyes.
7. Comprehensive Foot Exam
All individuals with diabetes should be screened for the presence of foot disease with a comprehensive foot exam at least once a year. The comprehensive foot exam should include inspection, assessment of pulses, and loss of sensation. The comprehensive foot exam may uncover high-risk foot diseases such as ulcers, infection, peripheral vascular disease (reduced circulation in the extremities), or peripheral neuropathy (nerve damage leading to loss of sensation in the feet).
Individuals with diabetes should inspect their feet on a daily basis for any injury. Foot injury increases the risk of lower extremity amputations. The ADA recommends an annual comprehensive foot exam to screen for the presence of diabetic foot disease. Other high-risk foot diseases include athlete’s foot (a fungal infection of the skin on the feet), fungal infections of the nails (onychomycosis), calluses, corns, bunions, blisters, dry skin, hammertoes, ingrown toenails, and warts on the bottom of the foot.
8. Dental Exam and Cleanings
All individuals with diabetes should have a dental exam with cleaning every 6-months. Research suggests individuals with diabetes are at higher risk for oral health problems such as gingivitis and periodontitis. Gingivitis is inflammation of the gums and represents the early stages of gum disease. Gingivitis can progress to periodontitis, a serious form of gum disease that can lead to painful chewing and even tooth loss.
Gum disease is largely preventable in individuals with diabetes. Gingivitis and periodontitis are usually the result of poor oral hygiene. Periodontitis in diabetics also increases the chances of heart attack, stroke, and other serious health problems. Control of blood glucose is both preventative and the primary treatment for gum disease. The American Dental Association recommends brushing at least twice a day and flossing daily. The American Diabetes Association (ADA) target goal for diabetics is healthy teeth and gums.
9. Influenza Vaccine
The influenza virus causes the flu. It is a serious disease that can lead to hospitalization and even death. As a result, the flu can have catastrophic effects on the health of a diabetic. Therefore, diabetics are considered a high-risk group with respect to influenza infection. The Advisory Committee on Immunization Practices (ACIP) advises vaccinating individuals at high risk before influenza season (September) each year. The influenza season can begin as early as October and last as late as May.
Influenza vaccination is the most effective measure for reducing the impact of influenza on diabetics and other high-risk groups. Both trivalent (three component) and quadrivalent (four component) injectable influenza vaccines are available. The US Centers for Disease Control and Prevention (CDC) recommends the nasal spray flu vaccine should not be used during 2016-2017.
10. Pneumonia Vaccine
The pneumonia vaccine can protect individuals with diabetes from contracting pneumonia caused by the bacteria Streptococcus pneumoniae, or pneumococcus. Pneumococcus can also cause ear and sinus infections, meningitis (infection of the meninges, which are the membranes surrounding the brain and spinal cord), and bacteremia (bloodstream infection) in adults and children. Pneumococcus is the most common cause of pneumonia, bloodstream infections, meningitis, and middle ear infections in young children.
Both the pneumococcal conjugate (PCV13 or Prevnar 13) and the pneumococcal polysaccharide (PPSV23 or Pneumovax) vaccines are available as injectables. PCV13 protects against 13-types of pneumococcal bacteria and is recommended in infants, young children, and all adults 65-years or older. PPSV23 protects against 23-types of pneumococcal bacteria and is recommended for all adults 65-years or older and children 2-years or older at high-risk for disease.