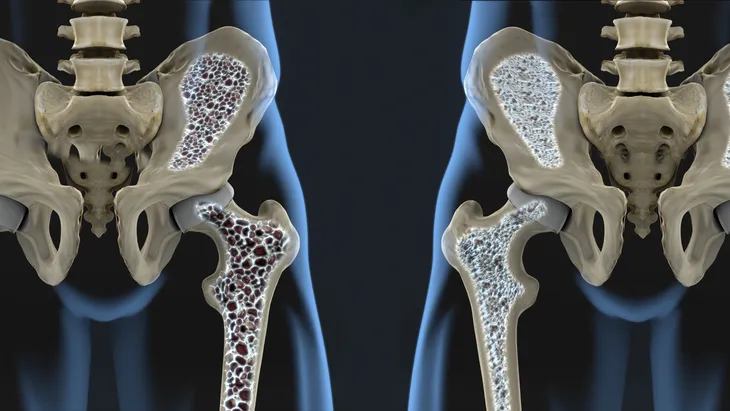
Osteoporosis is a disease characterized by the progressive thinning and weakening of bone, which is represented clinically by the loss of bone mass and density. The word literally means “porous bone.” According to the National Institutes of Health (NIH), more than 53-million individuals in the United States either have osteoporosis or are at high risk for developing the disease.
It is more common among the elderly, especially women. The disease increases the risk of fracturing bones, especially in the wrist, hip, and spine. Fractures due to osteoporosis can be disabling and can even greatly increase the risk of death.
Ten risk factors including the first sign of osteoporosis are…
Gender
Gender is a risk factor for osteoporosis that is uncontrollable. Women are 4-times more likely than men to develop osteoporosis. Women over the age of 50 have the greatest risk of developing the disease. According to the National Institute of Arthritis and Musculoskeletal and Skin Diseases, one of every two women over age 50 will likely have an osteoporosis-related fracture in their lifetime and 75-percent of all cases of hip osteoporosis affect women.
The higher risk for osteoporosis in women is a direct result of reduced estrogen levels at menopause. Estrogen is a hormone that helps regulate the menstrual cycle of women, but it also plays a role in keeping bones strong and healthy. The dramatic drop in estrogen production due to menopause translates into a significant loss of bone mass and density. In fact, the majority of the loss of bone mass in women occurs the in the years immediately after menopause.
Age
Age is another risk factor for osteoporosis that is uncontrollable. Osteoporosis is one of the most common conditions associated with aging. In general, men and women achieve maximum bone mass around age 30. After age 30, bone mass naturally begins to decline with age. As a result, the risk of developing osteoporosis increases with age. By about age 75, both men and women lose bone mass at the same rate.
Women and men over the age of 50 have the greatest risk of developing osteoporosis. According to the National Institute of Arthritis and Musculoskeletal and Skin Diseases, one of every two women and one in every four men over age 50 will likely have an osteoporosis-related fracture in their lifetime. Researchers from the Medical University of Vienna estimate 33-percent of community-dwelling individuals older than age 65 experience falls every year. The elderly with osteoporosis are at substantial risk for fractures with falls.
Ethnicity
Ethnicity is another risk factor for osteoporosis that is uncontrollable. Caucasian and Asian women are at the highest risk for the development of osteoporosis. According to the National Osteoporosis Foundation (NOF), an estimated 20-percent of Caucasian women and 20-percent of Asian women age 50 and older have osteoporosis. The NOF also estimates that 15-percent of Caucasian women and 90-percent of Asian women are lactose intolerant, which can make it difficult to get enough calcium for strong bones.
African-American and Hispanic women can develop osteoporosis, but are at less risk. According to the NOF, an estimated 5-percent of African-American women and 10-percent of Hispanic women age 50 and older have osteoporosis. An estimated 70-percent of African-American women are lactose intolerant. The differences in rates of osteoporosis among women of different ethnicities may be explained by research findings confirming that African-American and Hispanic women tend to have higher bone density throughout their lives.
Family History
Family history, or heredity, is one of the most important risk factors for the development of osteoporosis. It is also a risk factor for osteoporosis that is uncontrollable. An individual’s risk of osteoporosis is increased if one or more first-degree relatives (parent, sister, or brother) has the disease. The risk of osteoporosis is even greater if a first-degree relative has an osteoporosis-related fracture in the wrist, hip, or spine.
The United States Preventive Services Task Force recommends screening for osteoporosis in women age 65 or older, and earlier screening for women age 50-64 years with certain risk factors. For example, a 55-year old Asian woman whose parent had a hip fracture should consider early screening for osteoporosis. Researchers understand family history and osteoporosis to be a complex interplay of genetic, behavioral, and environmental factors.
Low Body Weight
Low body weight is a controllable risk factor for osteoporosis. Weighing less than 127-pounds or having a body mass index (BMI) less than 21-kilogram/meter increases the risk for the development of osteoporosis. BMI is calculated by dividing an individual’s weight in kilograms by the square of height in meters squared. BMI is an indirect measure to assess body fat and has been used for years to predict disease risk.
Women and men with a low body weight tend to have smaller bones, which translate into having less bone mass. Decreased bone mass combined with increased bone loss as an individual ages, further increases the risk of osteoporosis and fractures. In women, weight loss during the first few years after menopause causes even greater bone loss. Furthermore, individuals with low body weight have less fat around areas like the hips to cushion the impact of falls, which translates into an increased risk of fractures.
Smoking
Smoking cigarettes is another controllable risk factor for osteoporosis. Profound bone loss has been observed in older women and men who smoke. Researchers have shown a direct link between smoking and decreased bone density. The mechanism is poorly understood, but researchers suspect smokers may absorb less calcium from their diets. The nicotine in smoke and free radicals produced by smoking kill the bone producing cells called osteoblasts.
Compared to nonsmokers, women who smoke produce less of the sex hormone estrogen and tend to experience menopause earlier. Both factors may lead to increased bone loss. Furthermore, smoking damages blood vessels, which may translate into delayed healing of fractures deemed secondary to osteoporosis. Quitting smoking can reduce the risk of osteoporosis and fractures. The overall contribution of smoking to osteoporosis is complicated due to the fact that many individuals possess other risk factors that also increase the risk of osteoporosis.
Excessive Alcohol Consumption
Excessive alcohol consumption is another controllable risk factor for osteoporosis. Research has shown that regular consumption of more than two alcoholic drinks per day increases the risk of developing osteoporosis in men and women. Consuming more than four alcoholic drinks per day may double the risk of osteoporosis related fractures. In the United States, a standard drink is defined as 12-ounces of beer, 5-ounces of wine, or 1.5-ounces of distilled spirits.
Excessive alcohol consumption has a toxic effect upon bone forming cells. Osteoblasts are the cells responsible for the production of bone. Osteoclasts are the cells responsible for the breakdown of bone. As a result of alcohol’s toxic effect, individuals lose more bone mass, which leads to decreased bone density and an increased risk of fractures. Furthermore, excessive alcohol consumption increases the likelihood of falling, especially in the elderly. In turn, more falls increases the chances of fractures (hip, wrist, and spine) secondary to osteoporosis.
Medications
Medications are another controllable risk factor for the development of osteoporosis. Certain medications can lead to significant bone loss in men and women. Long-term use of steroids such as cortisone or prednisone may increase an individual’s risk of developing osteoporosis. Long-term use of steroid medication is defined as taking an oral dose of 5-mg or more for greater than 3-months. As a result, it is recommended to take steroids at the lowest possible dose for the shortest period of time to control symptoms.
In addition, the National Osteoporosis Foundation reports the following medicines may cause bone loss:
- Arimidex, Aromasin, Tamoxifen, and Femara, which are drugs used to treat breast cancer
- Phenytoin (Dilantin) and phenobarbital, which are antiseizure medications
- Heparin, a blood thinner
- Cyclosporine A, FK506 (Tacrolimus), and methotrexate, which are drugs that suppress the immune system
- Nexium, Prevacid, and Prilosec, which are drugs used to treat acid reflux
Note: The above list is not all-inclusive.
Chronic Diseases
Chronic diseases are another controllable risk factor for the development of osteoporosis. A variety of chronic diseases may increase an individual’s risk of developing osteoporosis. Rheumatoid arthritis, an inflammatory joint disease, may lead to bone loss. Research suggests the disease increases the activity of cells that breakdown bone, or osteoclasts. Other joint conditions that may increase the risk of osteoporosis include lupus, ankylosing spondylitis (spinal arthritis), psoriatic arthritis, and osteoarthritis.
Bowel diseases such as celiac disease, Crohn disease, and ulcerative colitis may affect the absorption of calcium and vitamin D, which are both vital to bone health. Hormonal diseases such as diabetes, hyperparathyroidism (overactive parathyroid glands), and hyperthyroidism (overactive thyroid gland) may lead to bone loss, which increases the likelihood of osteoporosis. Chronic kidney and chronic liver disease are associated with reduced bone formation. Chronic obstructive pulmonary diseases (COPD) such as emphysema and chronic bronchitis can also increase the risk of osteoporosis.
Lack of Exercise
Lack of exercise is another controllable risk factor for the development of osteoporosis. Studies have shown that women who sit for more than 9-hours per day are 50-percent more likely to have a hip fracture compared to those who sit less than 6-hours per day. Bone, like muscle, becomes stronger with exercise. The stress of exercise stimulates bone cell activity. Exercise also promotes balance, which can decrease the likelihood of falls and fractures.
Two types of exercises may help prevent osteoporosis: weight-bearing and muscle-strengthening exercises. Examples of high-impact weight-bearing exercises are dancing, hiking, jogging, and tennis. Examples of low-impact weight-bearing exercises are elliptical machines, stair-step machines, and walking on a treadmill. Examples of muscle-strengthening exercises are lifting free weights, using elastic exercise bands, and lifting one’s own body weight with pull-ups or push-ups. At least 30-minutes of exercise most days of the week, provides the greatest benefit to bone health.