The skin is the largest and one of the most complex organs of the body. Adults may suffer from a variety of skin disorders with tremendous variation in symptoms and severity. The causes of adult skin disorders may be genetic (hereditary), infectious, degenerative, or allergic. A great deal of adult skin disorders are benign (not life threatening), but some may be life threatening. Others may warrant referral to a dermatologist (a specialist in the treatment of skin disorders) for treatment that may entail medications, minor office procedures, or invasive surgery.
The twelve most common adult skin disorders are…
1. Acne
Acne is not solely restricted to adolescents and is a common condition among adults, especially females. Most individuals develop acne as an adolescent that persists into adulthood. A small portion of individuals may develop acne for the first time as an adult. Acne is characterized by pores clogged with oil and dead skin cells and may or may not be accompanied by inflammation. It may consist of whiteheads, blackheads, papules, pustules, cysts, or deep nodules.
Acne is strongly linked to hereditary factors, but may be made worse by fluctuating hormone levels, stress, hair and skin care products, medication side effects, or undiagnosed medical conditions. Most acne treatments are topical. Oral, or systemic, treatment is reserved for severe cases of acne and may be used in combination with topical treatments. Lastly, acne cases severely resistant to the combination of topical and oral treatments may be treated with minor office procedures.
2. Eczema
Eczema, also known as atopic dermatitis, is a common adult skin condition. The American Academy of Dermatology estimates 1 to 3-percent of adults have the condition. Most individuals develop the condition during childhood or adolescence and it persists into adulthood. Less often, it develops exclusively in adulthood. Inflamed, red, dry, and itchy patches of skin characterize eczema. The patches can occur anywhere on the body, but most commonly are seen on the elbows, hands, and in skin folds.
Eczema has strong genetic links and is commonly associated with asthma and hay fever (allergic rhinitis). It is estimated about 70-percent of individuals diagnosed with eczema have a family history of eczema, asthma, or hay fever. Eczema is not contagious. It has no cure, but may be controlled with topical steroid creams and ointments, oral antihistamines, and immunosuppressants (medications that prevent the immune system from overreacting). Particularly resistant cases of eczema may be treated with light therapy, or phototherapy.
3. Hives
Hives, also known as urticaria, are raised, red bumps (welts) that suddenly appear on the surface of the skin. The American College of Allergy, Asthma, and Immunology estimates the condition affects about 20-percent of individuals at some point in their lives. Hives can occur anywhere on the body. They are usually itchy, but can also sting or burn. Hives blanche, or turn white, when pressed. They vary in size from small to large and may coalesce, or come together, to form a very large mass.
Hives are usually caused by an allergic reaction to medications, foods, or food additives; but they may also be caused by bacterial infections (strep) and physical factors such as cold, exercise, or sunlight. They are usually acute (lasting < 6-weeks), but may be chronic (lasting > 6-weeks). Since chemicals called histamines drive many of the symptoms of hives, antihistamines provide effective relief.
4. Vitiligo
Vitiligo is a common adult skin condition in which an individual loses the pigment, or melanin, in their skin. Melanocytes are the cells in the skin responsible for the production of pigment. Vitiligo is characterized by the appearance of depigmented, or white, patches of skin due to loss of melanocytes. It usually occurs in areas of the skin exposed to sun such as the hands, face, arms, and feet.
The exact cause of vitiligo is unknown, but it is thought to represent an autoimmune disease. Autoimmune refers to the body attacking itself. The National Institute of Arthritis and Musculoskeletal and Skin Diseases estimates up to 30-percent of individuals diagnosed with the disorder have a family member with the same condition. Vitiligo cannot be cured and treatment is purely cosmetic. Treatment may options include topical steroids, ointments with immunomodulators (chemicals that interfere with the immune response), ultraviolet (UV) light therapy, or depigmentation of the rest of the body.
5. Psoriasis
Psoriasis is a common chronic adult skin condition characterized by thick, red patches or plaques of skin covered with white or silvery scales. Normally new skin cells takes weeks to form, but with psoriasis new skin cells form within days. The accelerated growth of new skin cells causes the accumulation of dead skin cells leading to the characteristic thick, red patches of the disease. The American Academy of Dermatology estimates 7.5-million Americans suffer with psoriasis.
The exact cause of psoriasis is unknown, but it is thought to represent an autoimmune response. Autoimmune refers to the body attacking itself. The patches of psoriasis most commonly appear on the elbows, knees, scalp, and lower back. Psoriasis has no cure, but can be effectively treated with various modalities including topical therapy, light therapy, and medications taken by mouth, injection, or IV to suppress the immune system.
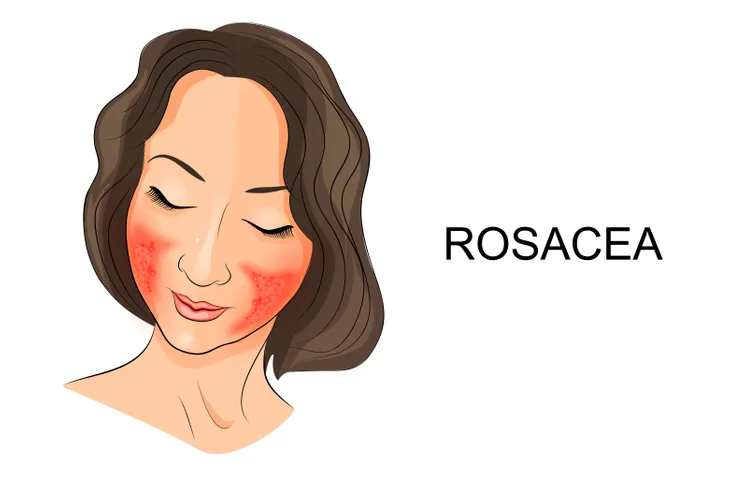
6. Rosacea
Rosacea is a chronic adult skin condition characterized by flushing and redness in the face. It most commonly occurs on the nose, chin, cheeks, and forehead. It less commonly may affect the eyes. The National Rosacea Society estimates 16-million Americans suffer with the disease. Thickened skin, pustules (pus-filled pimples), and enlargement of tiny blood vessels on the face may accompany rosacea. Alcohol, hot liquids, and spicy foods often precipitate the flushing of rosacea.
The exact cause of rosacea is unknown. There are four subtypes of rosacea. Risk factors for rosacea include age (30 to 50-years old), fair skin, Celtic or Scandinavian ancestry, female gender, and a family history of the disease. It occurs cyclically and is characterized by flare-ups. There is no cure for rosacea, but the symptoms may be minimized with treatments including topical and oral medications. Lasers may be used to treat enlargement of blood vessels on the face.
7. Athlete’s Foot
Athlete’s foot, also known as tinea pedis, is a fungal skin infection common among adults. Painful fissures (cracks), flaking, and peeling skin between the toes or side of the foot most commonly characterize the condition. Athlete’s foot is often pruritic, or itchy. Other symptoms may include burning or stinging in the area and blisters that ooze and eventually crust over. Tinea pedis can be a chronic infection that recurs frequently.
Athlete’s foot is spread through direct contact often in damp areas such as showers, locker rooms, and swimming pools. It is most commonly caused by the fungus Tricophyton rubrum, which thrives in warm, moist areas. According to the American Academy of Dermatology, tinea pedis is the most common fungal infection seen in developed countries. Over-the-counter or prescription topical antifungals are the mainstay of treatment for athlete’s foot. Oral antifungals may be considered for particularly resistant cases of tinea pedis.
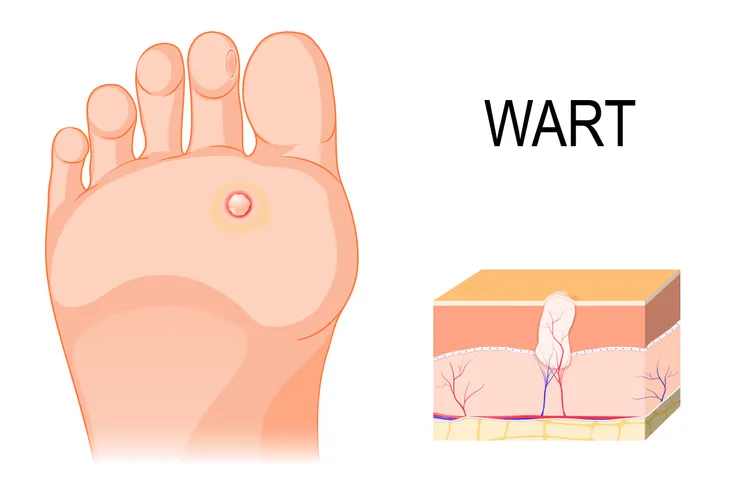
8. Warts
Warts are a common adult skin condition caused by the human papillomavirus, or HPV. There are more than 100-types of HPV. Warts are an ancient phenomenon and have been found on 3,000-year old mummies. They are flesh-colored, have a rough appearance, and may be flat or dome-shaped. Warts are most commonly found on the fingers, hands, arms, and feet. Less commonly, they are found in, on, or around the genitals. In women, genital warts can lead to cervical cancer.
Warts are benign (not cancerous) and painless. They are contagious and spread by direct contact, or sex in the case of genital warts. Warts may eventually resolve with no specific treatment, but it may take months to years. Using over-the-counter topical medications and freezing treatments can hasten the resolution of warts. Physicians may treat warts using a variety of methods including topical medications, freezing (cryotherapy), burning (electrosurgery), cutting out (excision), lasers, and chemical peels.
9. Skin Tags
Skin tags, also known as acrochorda (singular is acrochordon), are very common skin growths, or tumors. They are usually flesh-colored or slightly darker and hang from the skin by stalks. Skin tags may occur on the eyelids, neck, chest, back, armpits (axilla), under the breasts, or in the groin area. They are more common among women and the elderly. Individuals may have anywhere from one to hundreds of skin tags.
Almost everyone will develop a skin tag at some point in his or her lifetime. They are completely benign (not cancerous) and will not become cancerous if left untreated. Skin tags are not contagious. They sometimes fall off spontaneously, but most persist once formed. Treatment for skin tags may include freezing with liquid nitrogen (cryotherapy), tying off its base with a thread or suture, burning (electrocautery), or cutting off (excision) with scissors. There is no evidence that removing a skin tag will cause more to grow.
10. Moles
Moles, also known as nevi (singular is nevus), are very common skin growths. They usually appear as brown or black spots and can occur anywhere on the body. They can be smooth, wrinkled, flat or raised, and may have hair growing from them. Moles represent clusters of pigmented cells called melanocytes. They may appear during childhood, adolescence, and even adulthood. Almost every adult has a few moles, anywhere from 10 to 40 on his or her skin.
The majority of moles are benign (not cancerous), but rarely they can become melanoma (the most aggressive form of skin cancer). Suspicious moles may indicate melanoma, so individuals should look for asymmetrical shape; irregular borders; change in color; diameter greater than 6-millimeters; and evolving changes. Any moles that are painful, itch, burn, ooze, bleed, or show any of the ABCDE characteristics mentioned should immediately be evaluated by a dermatologist.
11. Shingles
Shingles, also known as herpes zoster, is a blistering rash commonly seen in older adults. It occurs when the dormant chickenpox, or varicella-zoster, virus is reactivated in nerve tissue. Early symptoms include pain or tingling on one side of the body or face, which is followed by red, blistering rash. The rash occurs on one side of the body and almost never crosses the midline. The rash usually resolves in 2 to 4-weeks.
Shingles has no cure, but prompt treatment can hasten healing and reduce the risk of complications. Prescription oral antiviral medications are the mainstay of shingles treatment. The pain, which can be severe, of shingles may be treated with numbing agents, narcotics, steroids, anticonvulsants, and even antidepressants. Common complications of shingles include skin infections and postherpetic neuralgia. Postherpetic neuralgia represents chronic nerve pain after the resolution of shingles and it develops in 20 to 30-percent of individuals.
12. Cold Sores
Cold sores, also known as fever blisters, are small, painful, fluid-filled blisters that occur on or around the mouth or nose. They are a common viral infection caused by the herpes simplex virus (HSV). Localized tingling and itching are the initial symptoms. Those symptoms are followed by an outbreak of blisters, often grouped together in patches. Once the blisters rupture, they crust over and heal without scarring. Cold sores typically take 2 to 4-weeks to resolve.
Cold sores are contagious and spread from person to person by direct contact, such as kissing. Individuals can spread HSV even without visible cold sores. Triggers for outbreaks of cold sores include stress, excess sun, fever, fatigue, viral infection, and hormonal changes (such as menstruation in females). There is no cure for cold sores, but treatment with over-the-counter creams and prescription oral antiviral drugs may speed the healing process.